Who We Are
At ForHealth Consulting, we partner with purposeful organizations to make healthcare and human services more equitable, effective, and accessible. As part of UMass Chan Medical School, we work with world-renowned faculty within a unique culture of collaboration to make lifesaving discoveries that help us advance together.
ForHealth Consulting leverages deep experience to create transformational solutions across the health and human services system, from payment and financing to clinical practice and information management.
Most of all, we believe in diversity and inclusion, and the power of a shared purpose; together, we can make healthcare better. Better for all of us.
Our State Partners and Our ForHealth Consulting Experts Presented At MESC!
We discussed solutions developed with state Medicaid partners to increase TPL benefits and savings.
Poster
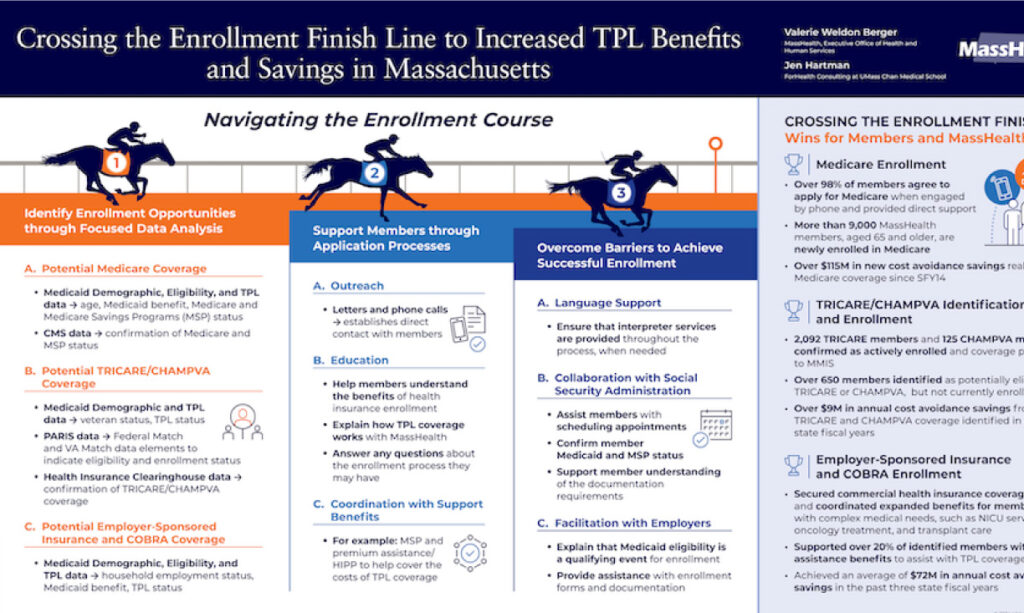
Crossing the Enrollment Finish Line to Increased TPL Benefits and Savings in Massachusetts
This poster highlights Massachusetts data analytics and enrollment support strategies to identify untapped TPL sources, assist members in navigating the health insurance enrollment course, and successfully cross the finish line to active TPL coverage, expanded benefits and savings.
Presentation
Crossing the Enrollment Finish Line: Increasing TPL Benefits in Massachusetts and Michigan
In this session, Massachusetts and Michigan shared Third Party Liability (TPL) data analytics and enrollment support strategies developed in collaboration with ForHealth Consulting to increase enrollment for Medicaid members in Medicare, TRICARE/CHAMPVA, and employer-sponsored insurance, expanding benefits for members and cost avoidance and recovery opportunities for states.
Our Services
Third Party Liability (TPL) Initiatives
Our team partners with states to help ensure Medicaid remains the Payer of Last Resort by providing specialized TPL initiatives that expand Medicare, TRICARE/CHAMPVA, and commercial health insurance coverage for members and savings opportunities for states.
Our services complement and supplement existing state TPL activities. We employ specialized analytical approaches and a deep understanding of state and federal rules and processes, combined with direct member support and proprietary software tools, to increase success. As a result, we achieved tens of millions of dollars in new cost avoidance savings for our state partners in the last fiscal year.
Our specialized TPL initiatives include:
Medicare Data Assurance Review
Using proprietary data integration and advanced data analysis techniques, we identify and validate new Medicare coverage information not previously updated in state Medicaid systems. Our consultants isolate and aid in resolving data discrepancies between federal and state data to improve the quantity and quality of Medicare data for cost avoidance and recovery activities. State partners have achieved tens of millions of dollars in cost savings resulting from newly identified and updated Medicare coverage.
Medicare Enrollment Support
Our team utilizes specialized data analysis to identify Medicaid members aged 65 and older who are potentially eligible for Medicare benefits. Then, we provide one-on-one member support through the Medicare enrollment process, resolving any barriers for members. When engaged and supported by our team, nearly all Medicaid members agree to apply for Medicare.
TRICARE/CHAMPVA Identification and Enrollment Support
Our experts assist states in identifying Medicaid recipients who may be eligible for insurance through TRICARE, a Department of Defense healthcare program, or CHAMPVA, a civilian health and medical program through the Department of Veterans Affairs. Using a comprehensive data analysis and outreach program, we help ensure that members can access TRICARE and CHAMPVA services and providers in addition to the Medicaid program.
Commercial TPL Consulting Services
Medicaid programs can see significant savings—tens of millions of dollars annually—if available private insurance covers costs for state Medicaid populations, especially for members with disabilities and chronic conditions who utilize high-cost services. Our consultants assist states in evaluating current commercial TPL activities, including health insurance identification and HIPP/premium assistance. We identify opportunities and provide recommendations for best practices to improve both the quantity and quality of TPL information, increasing commercial health insurance coverage and Medicaid savings. State partners achieve millions in annual cost savings resulting from new commercial insurance coverage opportunities identified through our commercial TPL initiatives.
Our Solutions
ForHealth is committed to finding solutions that transform healthcare. You need better access, better knowledge, and better performance for your organization and those you serve. Let’s get there together.
Better Access
Our healthcare system leaves too many behind. We help you put great care within reach of those who need it.
Better Knowledge
The right insights can make all the difference. We empower our partners with information that supports better outcomes.
Better Performance
Healthcare is complex. Our products make you more efficient, so you can deliver the right care where and when it matters.
Our Experts

Alda Rego MPA
Managing Director, Healthcare Finance Solutions
Alda Rego leads all health care finance cost avoidance and revenue recovery projects on behalf of municipal and state health care and public assistance programs. She oversees third party liability, health care reimbursement, program integrity and compliance, and state supplemental payment programs. In a previous role, she served as assistant secretary for administration and finance at the Massachusetts Executive Office of Health and Human Services.
Alda brings more than 20 years of experience delivering reliable, cost-saving solutions and strategies and successfully leading teams through key financial programs and services.
Jen Hartman
Deputy Director, Third Party Liability and Benefit Coordination
Jen Hartman leads an over 100-member team that provides health and human services operations, consulting, and customer service for state Medicaid programs, including identification of third-party resources, eligibility and enrollment, premium assistance, coordination of benefits, and recovery activities. She previously developed and implemented TPL initiatives to expand and coordinate benefits for Dually Eligible Medicaid-Medicare members.
Jen’s expertise and experience with state and federal data, combined with member support strategies and a collaborative approach to working with state Medicaid programs, SSA, and CMS, have achieved national and state-level successes for health and human services clients. This includes work resulting in member benefit expansions and two national benefit corrections that returned hundreds of millions of dollars to states.

Christopher Ciano, MS, BS
Associate Program Director, Medicare Eligibility Enhancement Program
Christopher Ciano manages multiple initiatives aimed at achieving Third Party Liability cost savings and revenue for one of ForHealth Consulting’s major Medicaid clients. He leads operations and consulting activities focused on identification, enrollment, and coordination of federal benefits for Medicaid members, including Medicare, Medicare Savings Programs, TRICARE, and CHAMPVA, provides oversight of the Medicare Buy-In program, administering payments of $70 million per month on behalf of more than 300,000 Medicaid members while ensuring efficiency, quality customer service, and compliance with state and federal laws.
Chris previously managed a State Health Insurance Assistance Program (SHIP) funded by the Centers for Medicare & Medicaid Services (CMS). He has more than 15 years of experience in Medicare and Medicaid administration and benefit coordination, data analysis, and state and federal program policies and regulations.
Kristin Lightbody, BS
Principal Director, Eligibility and Benefit Coordination Consulting
With a deep understanding of Medicaid eligibility, TPL, and benefit coordination, Kristin Lightbody leads a team of Medicaid eligibility subject matter experts in translating policy into system business requirements, implementing operational initiatives, and coordinating Medicaid eligibility and TPL processes for members.
As an expert in data analysis and program management, Kristin helps to deliver healthcare eligibility, financing, and policy solutions to advance innovation. She is currently leading the design, development, and implementation of Medicaid eligibility and program integrity initiatives, helping to achieve more accurate Medicaid benefit determinations across multiple eligibility systems and supporting tens of millions of dollars in cost savings to Medicaid clients.
Jeannette Lynch, BA
Director, Third Party Liability Programs
Jeannette Lynch manages and oversees health insurance identification and premium assistance, coordination of benefits, and TPL recovery operations, customer services, and special projects performed for state Medicaid clients.
Jeannette has more than 30 years of experience as a strategic leader in program development and deployment of TPL-related initiatives, as well as extensive knowledge of the Medicaid and Medicare programs, the commercial insurance industry, and Medicaid Management Information Systems.
Beth Nadeau, BA
Director, Medicare Eligibility Enhancement Programs
Beth Nadeau directs operations, customer service, and program development for initiatives focused on expanding eligibility for Medicare, Medicare Savings Programs (MSP), Social Security, and other federal benefits for state Medicaid populations and achieving enhanced cost savings and revenue opportunities for Medicaid programs. Beth has extensive experience working with state and federal data sets, identifying opportunities to expand and coordinating Medicare and other federal benefits, and developing collaborative efforts with Medicaid programs, SSA, and CMS to achieve results.
Beth has more than 25 years of experience in implementing and managing benefit coordination consulting projects and maximizing cost savings and revenue opportunities for Medicaid programs.
Matthew Hemberger, BS
Associate Director of Benefit Enrollment and Coordination, Third Party Liability Programs
Matthew Hemberger directs and oversees third party liability benefit coordination and premium assistance activities for state Medicaid clients with a focus on supporting benefit expansions for Medicaid members with disabilities and chronic conditions. Matthew leads initiatives to identify access to commercial health insurance options, including employer-sponsored insurance (ESI) and COBRA, through specialized data analysis and providing individualized support for Medicaid members through the enrollment process, including outreach and collaboration with employers and commercial insurers to overcome barriers and achieve successful enrollment and coordination of benefits.
Matthew is a public health administration professional with over 20 years of progressive experience in third party liability benefit coordination, revenue cycle, and patient access in both provider and payer roles to achieve financially sustainable healthcare delivery.
Our Work
Click on an image below to open link or download the file